

Association of the Work Schedules of Hospitalists With Patient Outcomes of Hospitalization. - PubMed - NCBI. Comfort Zone. The patient-doctor relationship may have a measurable positive impact on hospitalized patients’ care, according to a study published today in JAMA Internal Medicine.
The study, led by clinician researchers from Harvard Medical School and Beth Israel Deaconess Medical Center, reveals meaningful differences in care patterns and patient outcomes when hospitalized patients are treated by their own primary care physicians versus doctors with whom they do not have a prior relationship. Get more HMS news here. “We aimed to estimate differences in care and outcomes of hospitalized patients cared for by three different types of generalists,” said first author Jennifer P. Older patients seeing same GP each time 'key to reducing hospital admissions' Seeing the same GP each time they visit the doctor can reduce avoidable hospital admissions among older patients, a study published in the British Medical Journal has found.

But the government’s focus on increasing access to GPs, such as through longer hours, may have unintentionally affected the continuity of care patients experience, the authors warn. The study, by researchers at the Health Foundation charity, found that older patients who saw the same GP most of the time were admitted to hospital 12% less for conditions that could be treated in doctors’ surgeries than those who had a lower continuity of care. The compelling case for salaried physicians – canadianfemalesurgeon. It is a well known and accepted economic theory that once you get a minimal level above the poverty line in terms of household income, increasing levels of financial compensation are associated with decreasing returns on happiness.
When you go from a household income of $30000 a year to $60000- large increase in happiness. Double $60000 to $120000 and again your happiness level goes up. Just not as much as the original jump from $30000 to $60000. And so on. Simplifying Care for Complex Patients. Pcmh_evidence_report_FINAL. Margaret McCartney: There’s no magic GP production line. The new plan to save the NHS in England is for “every hospital A&E department” to have GP triage.
I’m a fan of GPs—after all, I am one. General practice is terrific, even when we’re not all wearing Wonder Woman bustiers. But this is another example of calamitous policy making. Firstly, GPs are not rabbits, which breed regularly, easily, and joyously. Does Loneliness Contribute to Morbidity and Mortality? By Katherine Otto Peer Reviewed What medications do you currently take?
Improving Clinical Access and Continuity through Physician Panel Redesign. British Journal of General Practice. How should continuity of care in primary health care be assessed? How primary care practices can improve continuity of care. Top evidence summary value of continuity. Family Doctors Who Do More, Save More. Is a good family doctor one who treats your knee pain and manages your recovery from heart surgery?
Or is it one who refers you to an orthopedist and a cardiologist? Those are questions at the heart of a debate about primary care – one with serious health and financial implications. Centre for Academic Primary Care. This calculator is designed to allow general practices to audit the levels of continuity of patient care provided in their practice.
It is intended to support the RCGP Continuity of Care Toolkit and the RCGP policy on Promoting Continuity of Care in General Practice The calculator is provided as a service to general practices. More Comprehensive Care Among Family Physicians is Associated with Lower Costs and Fewer Hospitalizations. + Author Affiliations CORRESPONDING AUTHOR: Andrew W.

Bazemore, MD, MPH, Robert Graham Center, 1133 Connecticut Avenue, NW Suite 100, Washington, DC 230036, ABazemore@aafp.org. Can micro-teams offer better continuity for multimorbidity in Tower Hamlets? Study affirms link between disjointed care and unnecessary medical procedures. A "look back" study of Medicare fee-for-service claims for more than 1.2 million patients over age 65 has directly affirmed and quantified a long-suspected link between lower rates of coordinated health care services and higher rates of unnecessary medical tests and procedures.

In a report on the study published online May 18 in JAMA Internal Medicine, a trio of Johns Hopkins researchers say they analyzed 5 percent of Medicare claims using a previously validated set of 19 over-used procedures and a measure of so-called continuity of care. Their results showed that 14.7 percent of patients were subjected to at least one potentially overused diagnostic, screening, monitoring or treatment procedure in 2008. Overall, patients who had more continuity in their medical care had a lower chance of having an overused procedure. For the study, Romano and his colleagues measured the number of procedures each Medicare patient received that could be classified as potentially overused.
The Association Between Continuity of Care and the Overuse of Medical Procedures. Importance Both the overuse of unnecessary medical procedures and poor continuity of care are thought to contribute to high health care spending and poor patient outcomes.
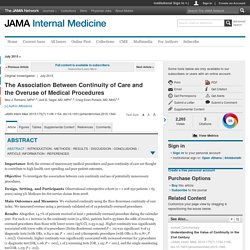
Objective To investigate the association between care continuity and use of potentially unnecessary procedures. Design, Setting, and Participants Observational retrospective cohort (n = 1 208 250 patients > 65 years) using 5% Medicare fee-for-service claims from 2008. Main Outcomes and Measures We evaluated continuity using the Bice-Boxerman continuity of care index. The impact of hospitalist discontinuity on hospital cost, readmissions, and patient satisfaction. Association Between End-of-Rotation Resident Transition in Care and Mortality Among Hospitalized Patients. Question Are patients who are exposed to end-of-rotation resident transition in care at risk for greater mortality, and is this association related to the 2011 duty-hour regulations? Findings In this multicenter cohort study of 230 701 patients admitted to internal medicine services in 10 Veterans Affairs hospitals, end-of-rotation house staff transition in care was associated with significantly higher in-hospital mortality (3.5% for intern only transition vs 2.0% for control and 4.0% for intern + resident transition vs 2.1% for control).
The association was significantly stronger following institution of ACGME duty hour regulations. Meaning End-of-rotation transitions may introduce risk in internal medicine inpatient care. Importance Shift-to-shift transitions in care among house staff are associated with adverse events. Providing continuity of care to a specific population. Objective To analyze the factors that influence newly licensed family physicians in their decision to provide continuity of care to a specific primary care population.
Design Mixed-methods study that included a self-administered online questionnaire for family physicians followed by individual interviews. Setting Monteregie, the second-most populated region of Quebec, with rural and urban areas. Participants All family physicians with 10 or fewer years of work experience who were practising in Monteregie were contacted (366 physicians). Of this group, 118 completed the online questionnaire (response rate of 32.2%). Geography vs. continuity. Published in the March 2017 issue of Today’s Hospitalist INCREASINGLY, unit-based care is considered the gold standard that hospitalist groups should at least try to attain.
But the hospitalist group I direct has spent the past year unwinding a geographic model that had long been in place. Association of weekend continuity of care with hospital length of stay. A prospective cohort study found that provider and information. Frail elderly patients. New model for integrated service delivery. A systematic review of nurse-assisted case management to improve hospital discharge transition outcomes for the elderly.
Integrated care for frail elderly compared to usual care: a study protocol of a quasi-experiment on the effects on the frail elderly, their caregiver... Brief hospitalizations of elderly patients: a retrospective, observational study. A structured review of chronic care model components supporting transition between healthcare service delivery types for older people with multiple c... Frequent Use of Emergency Departments by the Elderly Population When Continuing Care Is Not Well Established.