

Does COVID‐19 contribute to development of neurological disease? - Mahalakshmi - 2021 - Immunity, Inflammation and Disease. Coronavirus disease-19 (COVID-19) was first identified in Wuhan, China, in early December 2019.

In the past few months, this pandemic disease had spread all over the world and caused over 38,925,204 confirmed infections, with 1,098,378 fatal cases globally as of 16 October 2020, according to the Johns Hopkins University dashboard. Coronaviruses (CoVs) are not new. The first described coronavirus was isolated from chickens in 1937. Human coronaviruses (HCoVs) were first found to be pathogenic in the mid-1960s by Tyrrell and Bynoe.1, 2 HCoVs received more attention globally during the 2002-2003 outbreak of severe acute respiratory syndrome (SARS) by SARS-CoV, and the Middle East respiratory syndrome coronavirus (MERS-CoV) outbreak in 2012. Supercomputer Simulations Reveal How Dominant COVID-19 Strain Binds to Host, Succumbs to Antibodies.
Supercomputer simulations at Los Alamos National Laboratory demonstrated that the G form of SARS-CoV-2, the dominant strain of the virus causing COVID-19, mutated to a conformation that allows it to more easily attach to host receptors, while also being more susceptible to antibodies than the original D form.
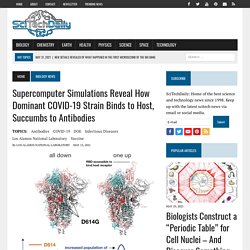
Credit: Los Alamos National Laboratory Dominant G-form Spike protein ‘puts its head up’ more frequently to latch on to receptors, but that makes it more vulnerable to neutralization. Large-scale supercomputer simulations at the atomic level show that the dominant G form variant of the COVID-19-causing virus is more infectious partly because of its greater ability to readily bind to its target host receptor in the body, compared to other variants. These research results from a Los Alamos National Laboratory–led team illuminate the mechanism of both infection by the G form and antibody resistance against it, which could help in future vaccine development.
The SARS-CoV-2 Spike variant D614G favors an open conformational state. Abstract The COVID-19 (coronavirus disease 2019) pandemic underwent a rapid transition with the emergence of a dominant viral variant (from the “D-form” to the “G-form”) that carried an amino acid substitution D614G in its “Spike” protein.

The G-form is more infectious in vitro and is associated with increased viral loads in the upper airways. To gain insight into the molecular-level underpinnings of these characteristics, we used microsecond all-atom simulations. We show that changes in the protein energetics favor a higher population of infection-capable states in the G-form through release of asymmetry present in the D-form inter-protomer interactions. Thus, the increased infectivity of the G-form is likely due to a higher rate of profitable binding encounters with the host receptor. Ferrets, Cats, Civets, and Dogs Most Susceptible to SARS-CoV-2 Coronavirus Infection After Humans. In blue, the human ACE2 protein and in grey, the coronavirus spike protein.
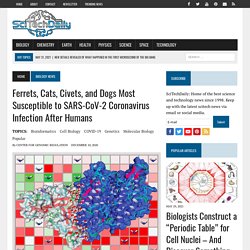
Pictured are how the two proteins interact in a lock-and-key mechanism, which allows the virus to enter the cell and hijack its protein-making machinery to replicate itself. Credit: Javier Delgado Ducks, rats, mice, pigs, and chickens had lower or no susceptibility to infection. Humans, followed by ferrets and to a lesser extent cats, civets and dogs are the most susceptible animals to SARS-CoV-2 infection, according to an analysis of ten different species carried out by researchers at the Centre for Genomic Regulation (CRG), based in Barcelona.
“You Do Not Want to Mess With This Virus” – Research Strongly Suggests COVID-19 Virus Enters the Brain. The S1 protein likely causes the brain to release inflammatory products causing a storm in the brain, researchers said.

Credit: Alice Gray A study published in Nature Neuroscience shows how spike protein crosses the blood-brain barrier. More and more evidence is coming out that people with COVID-19 are suffering from cognitive effects, such as brain fog and fatigue. The S1 protein of SARS-CoV-2 crosses the bloodâbrain barrier in mice. Mice All mouse studies were approved by the local Institutional Animal Care and Use Committee at Oregon Health & Sciences University and the Veterans Affairs Puget Sound Health Care System (VAPSHCS) and conducted in facilities approved by the American Association for Accreditation of Laboratory Animal Care (AAALAC).

Male CD-1 mice (6–10 weeks old) were purchased from Charles River Laboratories (Hollister). Clinical Characteristics and Disease Severity Among Infants With SARS-CoV-2 Infection in Montreal, Quebec, Canada. With more than 40 million cases of confirmed severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection worldwide, the clinical presentation and risk factors for disease severity among adults and children have now been well described.1 SARS-CoV-2 is the virus that causes coronavirus disease 2019.
However, little remains known about disease manifestation and severity of illness in infants.2 Although infants are at higher risk of severe disease and complications from other common viral respiratory pathogens (influenza, respiratory syncytial virus), it is not yet clear whether this is the case with SARS-CoV-2 infection because few series describing outcomes in infants have been published.3,4 The objective of this study was to describe the manifestations and severity of disease among infants with SARS-CoV-2 infection. Table 1 describes clinical manifestations and disease severity among all infants.
Disease was mild in most cases (24 infants [89%]) of cases. The Coronavirus Killed the Gospel of Small Government. This is the story of so much of what went wrong last year.
Doctors and nurses were left without basic protective equipment because the United States lacked the manufacturing capacity to produce it. Efforts to track and contain the virus were delayed by bottlenecks in test production and shortages of supplementary equipment like swabs. Once tests could be administered, a nationwide scarcity of test-processing equipment prolonged the delivery of test results. The reason: More than a decade into a hospital-closure crisis, the United States faced a shortage of beds and medical facilities necessary to manage an emergency. Hospitals overrun with Covid-19 patients turned away ambulances. ViewSpecialArticleDetail. Europe: coronavirus cases by day. IFCN Covid-19 Misinformation. Who are the doctors in the viral hydroxychloroquine video? Despite social media platforms’ efforts to remove it, millions of people have seen a viral video of doctors making false and misleading claims about the coronavirus pandemic.

Breitbart, a conservative news outlet, published the 40-plus-minute-long video on Facebook, Twitter and YouTube on July 27. It’s a live stream of a Washington, D.C., press conference organized by the Tea Party Patriots, a conservative group backed by Republican donors. Artificial intelligence model detects asymptomatic Covid-19 infections through cellphone-recorded coughs. Asymptomatic people who are infected with Covid-19 exhibit, by definition, no discernible physical symptoms of the disease.
They are thus less likely to seek out testing for the virus, and could unknowingly spread the infection to others. But it seems those who are asymptomatic may not be entirely free of changes wrought by the virus. MIT researchers have now found that people who are asymptomatic may differ from healthy individuals in the way that they cough. Responding to Covid-19 — A Once-in-a-Century Pandemic? In any crisis, leaders have two equally important responsibilities: solve the immediate problem and keep it from happening again. The Covid-19 pandemic is a case in point. We need to save lives now while also improving the way we respond to outbreaks in general. The first point is more pressing, but the second has crucial long-term consequences.
The long-term challenge — improving our ability to respond to outbreaks — isn’t new. Update: ‘A bit chaotic.’ Christening of new coronavirus and its disease name create confusion. *Update, 13 February, 12:15 p.m.: The story below, published on 12 February, has been updated with information from a WHO spokesperson. “COVID-19. I’ll spell it: C-O-V-I-D hyphen one nine.
COVID-19.” That’s how Tedros Adhanom Ghebreyesus, head of the World Health Organization (WHO), introduced the agency’s official name for the new disease that’s paralyzing China and threatening the rest of the world. Strategic intelligence: COVID-19.