

Oxygen equivalent. Oxygen equivalent compares the relative amount of oxygen available for respiration at a variable pressure to that available at SATP.

As external respiration depends on the exchange of gases due to partial pressures across a semipermeable membrane and normally occurs at SATP, an oxygen equivalent may aid in recognizing and managing variable oxygen availabiity during procedures such as hyperbaric oxygen therapy or medical air transport. It does so by expressing oxygen concentration as a ratio of the partial pressure of oxygen at a given altitude or pressure to Standard Atmospheric Pressure; rather than as a ratio of the PO2 at a given pressure to the total pressure of the gas mixture. The latter would generally be 0.2095, the atmospheric concentration by volume of O2, although FO2 and Patm vary for extraterrestrials. Calculations occur as follows: O2E = FO2(Pb + dP)/ Patm It is worthwhile to note that pressures may often be expressed in units of distance such as feet when diving.
Pulmonology. Pulmonology is a medical specialty that deals with diseases involving the respiratory tract.[1] The term is derived from the Latin word pulmō, pulmonis ("lung") and the Greek -λογία, -logia.
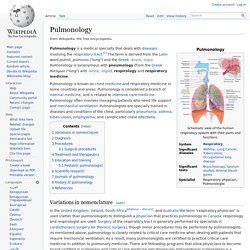
Pulmonology is synonymous with pneumology (from the Greek πνεύμων ("lung") and -λογία, -logia), respirology and respiratory medicine. Pulmonology is known as chest medicine and respiratory medicine in some countries and areas. Pulmonology is considered a branch of internal medicine, and is related to intensive care medicine. Pulmonology often involves managing patients who need life support and mechanical ventilation.
Exsufflation. Exsufflation is a strongly forced expiration of air.
In medicine, airway secretions can be cleared with manual and mechanical exsufflation. Mechanical insufflation-exsufflation devices (also known as In-Exsufflator, Cofflator, and cough machine) alternate positive and negative airway pressure to stimulate cough. It is typically used in patients with neuromuscular disorders and sleep apnea.[1] After certain surgical procedures, the gases (such as carbon dioxide) used to expand body cavities are mechanically or manually exsufflated.
The term is also used of certain rituals in the Christian religion involving the blowing of air to remove evil spirits; these survive in Eastern Christianity, but between the sixteenth and twentieth centuries were progressively abandoned in the West. For details see Insufflation. Müller's maneuver. Müller's Manoeuvre After a forced expiration, an attempt at inspiration is made with closed mouth and nose, whereby the negative pressure in the chest and lungs is made very subatmospheric; the reverse of Valsalva manoeuvre.
This technique is designed to look for collapsed sections of airways such as the trachea and upper airways. In this maneuver, the patient attempts to inhale with his mouth closed and his nostrils plugged, which leads to a collapse of the airway.
Breathing set. A breathing set may refer to:

Timeline of respiratory therapy. From Wikipedia, the free encyclopedia Ancient period[edit] 1550 BC: (EG) The Ebers Papyrus describes ancient Egyptian inhalation treatments for asthma.
Ventilation. Respiratory examination. Liquid breathing. Perfluorochemical (perfluorocarbon) molecules have very different structures that impart different physical properties such as respiratory gas solubility, density, viscosity, vapor pressure, and lipid solubility.[1] Thus, it is critical to select the appropriate PFC for a specific biomedical application, such as liquid ventilation, drug delivery or blood substitutes.

The physical properties of PFC liquids vary substantially; however, the one common property is their high solubility for respiratory gases. In fact, these liquids carry more oxygen and carbon dioxide than blood.[2]
Physiology of respiratory. Bronchoscopy. Bronchoscopy is an endoscopic technique of visualizing the inside of the airways for diagnostic and therapeutic purposes.

An instrument (bronchoscope) is inserted into the airways, usually through the nose or mouth, or occasionally through a tracheostomy. This allows the practitioner to examine the patient's airways for abnormalities such as foreign bodies, bleeding, tumors, or inflammation. Specimens may be taken from inside the lungs. The construction of bronchoscopes ranges from rigid metal tubes with attached lighting devices to flexible optical fiber instruments with realtime video equipment. History[edit] A German, Gustav Killian, performed the first bronchoscopy in 1897. An American, Chevalier Jackson, refined the rigid bronchoscope in the 1920s, using this rigid tube to visually inspect the trachea and mainstem bronchi.
Carbon dioxide scrubber. A carbon dioxide scrubber is a device which absorbs carbon dioxide (CO2).
It is used to treat exhaust gases from industrial plants or from exhaled air in life support systems such as rebreathers or in spacecraft, submersible craft or airtight chambers. Carbon dioxide scrubbers are also used in controlled atmosphere (CA) storage. Technologies[edit] Respiratory Care Week. Respiratory Care Week is a week set to honor and recognize respiratory therapists.
Respiratory Care Week is celebrated internationally but most notably in Canada and the United States. Respiratory Care Week is usually the last full week of October.[1] United States President Ronald Reagan proclaimed the first week dedicated to honoring respiratory therapists in 1982. Originally November 7 through November 13, 1982[2][3] Previous dates[edit] 1982: November 7 — November 131983: September 15 — October 12011: October 23 — October 29.
Valsalva maneuver. The Valsalva maneuver or Valsalva manoeuvre is performed by moderately forceful attempted exhalation against a closed airway, usually done by closing one's mouth, pinching one's nose shut while pressing out as if blowing up a balloon. Variations of the maneuver can be used either in medical examination as a test of cardiac function and autonomic nervous control of the heart, or to "clear" the ears and sinuses (that is, to equalize pressure between them) when ambient pressure changes, as in diving, hyperbaric oxygen therapy, or air travel. The technique is named after Antonio Maria Valsalva,[1] a 17th-century physician and anatomist from Bologna whose principal scientific interest was the human ear. He described the Eustachian tube and the maneuver to test its patency (openness).
Pulmonology. High-altitude pulmonary edema. High-altitude pulmonary edema (HAPE) (HAPO spelled oedema in British English) is a life-threatening form of non-cardiogenic pulmonary edema (fluid accumulation in the lungs) that occurs in otherwise healthy mountaineers at altitudes typically above 2,500 meters (8,200 ft).[1] Some cases, however, have been reported also at lower altitudes (between 1,500–2,500 metres or 4,900–8,200 feet in highly vulnerable subjects), although what makes some people susceptible to HAPE is not currently known.
HAPE remains the major cause of death related to high-altitude exposure, with a high mortality rate in the absence of adequate emergency treatment. Symptoms[edit] Physiological and symptomatic changes often vary according to the altitude involved.[2] The Lake Louise Consensus Definition for High-Altitude Pulmonary Edema has set widely used criteria for defining HAPE symptoms:[3] Symptoms: at least two of: