

Could I Have Lupus? : How to Get Help. Dermatology A to Z. Discoid Lupus Erythematosus. Steroids (Topical) Steroids (Oral) Many of the symptoms of skin disease result from inflammation in tissues of the body.
Cortisone, manufactured naturally by the body's adrenal glands and also made synthetically, has been found to have a marked anti-inflammatory effect. Cortisone and its derivatives are steroids, among the most effective anti-inflammatory drugs known. Their use can substantially reduce the swelling, warmth, tenderness and pain that are associated with inflammation. While steroid dosage should be kept at the lowest effective level, steroids must not be stopped suddenly if they have been taken for more than four weeks.
By this time, some shrinking of the adrenal glands will occur, as their burden of producing cortisone has been relieved. Steroids may be given as a pill, by intra-muscular (IM) injection or may be injected directly into the skin. Prednisone is the oral tablet form of steroid most often used. Prednisone is an extremely effective drug and may be necessary for control. Back to Index. Intralesional Injection. Cutaneous lupus erythematosus. DermNet NZ. Facts about the skin from DermNet New Zealand Trust.

Topic index: A B C D E F G H I J K L M N O P Q R S T U V W X Y Z Lupus erythematosus (LE) of the skin comprises an uncommon group of skin disorders. They most often affect young adult women (aged 20 to 50) but children, the elderly, and males may be affected. What causes lupus erythematosus? LE is classified as autoimmune, as it is associated with antibodies directed against components of cell nuclei. There are various types of cutaneous LE. Discoid lupus erythematosus In the most common form, discoid LE, unsightly red scaly patches develop which leave postinflammatory pigmentation and white scars. Discoid LE predominantly affects the cheeks, nose and ears, but sometimes involves the upper back, V of neck, and backs of hands. Subacute lupus erythematosus In subacute LE, a non-itchy dry rash appears on the upper back and chest, often following sun exposure. Hair loss, balding, hair shedding, alopecia. DermNet NZ. Facts about the skin from DermNet New Zealand Trust.
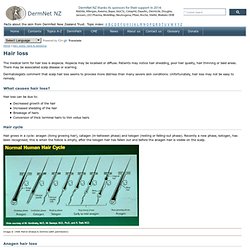
Topic index: A B C D E F G H I J K L M N O P Q R S T U V W X Y Z The medical term for hair loss is alopecia. Alopecia may be localised or diffuse. Patients may notice hair shedding, poor hair quality, hair thinning or bald areas. There may be associated scalp disease or scarring. Dermatologists comment that scalp hair loss seems to provoke more distress than many severe skin conditions. What causes hair loss? Hair loss can be due to: Decreased growth of the hair Increased shedding of the hair Breakage of hairs Conversion of thick terminal hairs to thin vellus hairs Hair cycle Hair grows in a cycle: anagen (living growing hair), catagen (in-between phase) and telogen (resting or falling-out phase).
Image © 1998 Merck Sharpe & Dohme (with permission) Postinflammatory hyperpigmentation. DermNet NZ. Facts about the skin from DermNet New Zealand Trust.
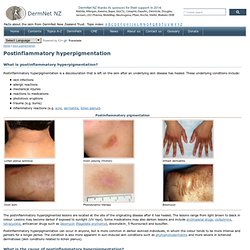
Topic index: A B C D E F G H I J K L M N O P Q R S T U V W X Y Z What is postinflammatory hyperpigmentation? Postinflammatory hyperpigmentation is a discolouration that is left on the skin after an underlying skin disease has healed. These underlying conditions include: skin infections allergic reactions mechanical injuries reactions to medications phototoxic eruptions trauma (e.g. burns) inflammatory reactions (e.g. acne, dermatitis, lichen planus). The postinflammatory hyperpigmented lesions are located at the site of the originating disease after it has healed. Postinflammatory hyperpigmentation can occur in anyone, but is more common in darker skinned individuals, in whom the colour tends to be more intense and persists for a longer period.
What is the cause of postinflammatory hyperpigmentation? What is the treatment for postinflammatory hyperpigmentation? These treatments are not effective in dermal hypermelanosis. Discoid Lupus Erythematosus. What is discoid lupus erythematosus?
Discoid lupus erythematosus is an autoimmune disorder affecting the skin. The disorder causes a skin rash or lesions that usually appear on the nose and cheeks. Loss of hair and changes in skin pigment also occur with this disorder. Autoimmune Disease Spotlight Discoid lupus erythematosus is more common in women than men and appears to have a familial linkage. Discoid Lupus Erythematosus. Early Diagnosis and Treatment of Discoid Lupus Erythematosus. Suresh Panjwani, MD, MSc, FRACGP + Author Affiliations Corresponding author: Suresh Panjwani, MD, MSc, FRACGP, 4 Harper Close, Southgate, London N14 4ES, United Kingdom (E-mail: sureshpanjwani18@hotmail.com) Abstract Discoid lupus erythematosus is a chronic dermatological disease that can lead to scarring, hair loss, and hyperpigmentation changes in skin if it is not treated early and promptly.

It has a prolonged course and can have a considerable effect on quality of life. Lupus erythematosus (LE) is thought to be an autoimmune disease among other connective tissue diseases like scleroderma, rheumatoid arthritis, polymyositis, and mixed connective tissue disease. The diagnosis of discoid lupus is generally made based on clinical features. DLE tends to run a less severe course than SLE and has a better prognosis. Clinical Features.