

Brain herniation. Herniation can also occur in the absence of high ICP when mass lesions such as hematomas occur at the borders of brain compartments.
In such cases local pressure is increased at the place where the herniation occurs, but this pressure is not transmitted to the rest of the brain, and therefore does not register as an increase in ICP.[2] Because herniation puts extreme pressure on parts of the brain and thereby cuts off the blood supply to various parts of the brain, it is often fatal. Therefore, extreme measures are taken in hospital settings to prevent the condition by reducing intracranial pressure, or decompressing (draining) a hematoma which is putting local pressure on a part of the brain. Classification[edit] Types of brain herniation[3] 1) Uncal 2) Central 3) Cingulate 4) Transcalvarial 5) Upward 6) Tonsillar There are two major classes of herniation: supratentorial and infratentorial. Brain (Human Anatomy): Picture, Function, Parts, Conditions, and More.
Bitemporal hemianopsia. Optic disk. Papilledema – Pictures, Definition, Causes, Symptoms and Treatment. Are constant headaches ruining your days?
Having a nauseating feeling and a vomiting sensation? You may be suffering from Papilledema, a condition that affects the optic disc. Papilledema Definition Picture 1 – PapilledemaSource – eyeweb Doctors and medical researchers define Papilledema as a medical condition that affects the eyes of a person. This medical syndrome affects about 200,000 people only in the United States. Papilledema Symptoms Swelling of the optic nerves is not the only symptom of Papilledema. Headache The patient experiences constant pain in the head.
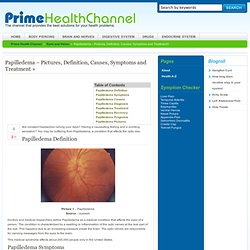
Nausea The affected person also suffers from a nauseating feeling that makes the head reel. Vomiting The sufferer also has a vomiting sensation from time to time that impairs his or her daily activities. Short-Term Vision Loss Vision loss is one of the most notable Papilledema signs. Reduced Scope of Vision The area of vision narrows down in suffering persons. Changes in Vision. Intracranial hemorrhage. Subarachnoid hemorrhage. Symptoms of SAH include a severe headache with a rapid onset ("thunderclap headache"), vomiting, confusion or a lowered level of consciousness, and sometimes seizures.[1] In general, the diagnosis is confirmed with a CT scan of the head, or occasionally by lumbar puncture.
Treatment is by prompt neurosurgery or radiologically guided interventions with medications and other treatments to help prevent recurrence of the bleeding and complications. Surgery for aneurysms was introduced in the 1930s, but since the 1990s many aneurysms are treated by a less invasive procedure called "coiling", which is carried out by instrumentation through large blood vessels.[1] SAH is a form of stroke and comprises 1–7 percent of all strokes.[2] It is a medical emergency and can lead to death or severe disability—even when recognized and treated at an early stage.
Signs and symptoms[edit] Google Image Result for. Subarachnoid hemorrhage imaging ct. Subarachnoid Hemorrhage. When a cerebral aneurysm ruptures, blood will fill the space surrounding the brain.
Subarachnoid hemorrhage occurs when a blood vessel just outside the brain ruptures. The area of the skull surrounding the brain (the subarachnoid space) rapidly fills with blood. File:Subdural-hematoma-102.jpg - RadsWiki. Welcome to LearningRadiology - radiology, radiologic, imaging, signs, list, collection, illustrated, cases, xray, x-ray, gi, gu, chest, thoracic, teaching, website, web, site. Subdural Hematoma - Medical Illustration, Human Anatomy Drawing, Anatomy Illustration.
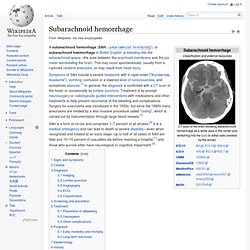
Subdural Hematoma - Topic: 809 from the MedPix® Medical Image Database. Spinal Cord - Figure 3 for article: Papilloedema in association with spinal lipoma and bilateral chronic subdural bleeding. Left subdural compartment hemorrhage. a T1-W coronal MR image shows left subdural compartment hemorrhage. b Graphic representation of hemorrhage originating from the inner dural plexus (BV bridging vein, DP dural plexus) Imaging in Epidural Hematoma.
Because of the need for accurate and rapid diagnosis and treatment, prompt transfer of the patient to a facility capable of computed tomography (CT) scanning and neurosurgical intervention is necessary.
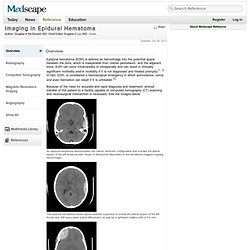
See the images below. An epidural hematoma demonstrates the classic lenticular configuration that overlies the lateral aspect of the left temporal lobe. Areas of diminished attenuation in the hematoma suggest ongoing hemorrhage. The epidural hematoma shown above extends superiorly to overlie the lateral aspect of the left frontal lobe with associated sulcal effacement, as well as a rightward midline shift of 5-6 mm.
An epidural hematoma overlies the right frontal lobe with right-to-left subfalcine herniation of approximately 7 mm. Atherosclerosis and Ischaemic Stroke. Transient ischemic attack. A transient ischemic attack (TIA) is a transient episode of neurologic dysfunction caused by ischemia (loss of blood flow) – either focal brain, spinal cord or retinal – without acute infarction (tissue death).
TIAs have the same underlying cause as strokes: a disruption of cerebral blood flow (CBF), and are frequently referred to as mini-strokes. TIAs cause the same symptoms associated with stroke, such as contralateral paralysis (opposite side of body from affected brain hemisphere) or sudden weakness or numbness. A TIA may cause sudden dimming or loss of vision (amaurosis fugax), aphasia, slurred speech (dysarthria) and mental confusion. But unlike a stroke, the symptoms of a TIA can resolve within a few minutes or 24 hours. Brain injury may still occur in a TIA lasting only a few minutes. A cerebral infarct that lasts longer than 24 hours but fewer than 72 hours is called a reversible ischemic neurologic deficit or RIND.
Signs and symptoms[edit] Causes[edit] Amaurosis fugax: MedlinePlus Medical Encyclopedia. Amaurosis fugax is loss of vision in one eye due to a temporary lack of blood flow to the retina.

It may be a sign of an impending stroke. See: Stroke risk factors and prevention. Amaurosis fugax. Amaurosis fugax (Latin fugax meaning fleeting, Greek amaurosis meaning darkening, dark, or obscure) is a painless transient monocular visual loss (i.e., loss of vision in one eye that is not permanent).[1] Pathophysiology and etiology[edit] Embolic and hemodynamic origin[edit] With respect to embolic and hemodynamic causes, this transient monocular visual loss ultimately occurs due to a temporary reduction in retinal artery, ophthalmic artery, or ciliary artery blood flow, leading to a decrease in retinal circulation which, in turn, causes retinal hypoxia.[5] While, most commonly, emboli causing amaurosis fugax are described as coming from an atherosclerotic carotid artery, any emboli arising from vasculature preceding the retinal artery, ophthalmic artery, or ciliary arteries may cause this transient monocular blindness.

Ocular origin[edit] Ocular causes include: Neurologic origin[edit] Neurological causes include: Google Image Result for. Google Image Result for. Google Image Result for. Google Image Result for. Lacunar infarcts. Google Image Result for. Alzheimer's disease. How the Brain and Nerve Cells Change During Alzheimer's Disease. Brain With Alzheimer's Disease. Prion Diseases. Prion diseases or transmissible spongiform encephalopathies (TSEs) are a family of rare progressive neurodegenerative disorders that affect both humans and animals.
They are distinguished by long incubation periods, characteristic spongiform changes associated with neuronal loss, and a failure to induce inflammatory response. The causative agents of TSEs are believed to be prions. The term "prions" refers to abnormal, pathogenic agents that are transmissible and are able to induce abnormal folding of specific normal cellular proteins called prion proteins that are found most abundantly in the brain.
The functions of these normal prion proteins are still not completely understood. The abnormal folding of the prion proteins leads to brain damage and the characteristic signs and symptoms of the disease. Listed below are the prion diseases identified to date. Human Prion Diseases Animal Prion Diseases Surveillance for human disease is primarily the responsibility of CDC.