

Respirometer. A simple whole plant respirometer designed to measure oxygen uptake or CO2 release consists of a sealed container with the living specimen together with a substance to absorb the carbon dioxide given off during respiration, such as soda lime pellets or cotton wads soaked with potassium hydroxide.

The oxygen uptake is detected by manometry. Typically, a U-tube manometer is used, which directly shows the pressure difference between the container and the atmosphere. Exhaled nitric oxide. Chemical formula of nitric oxide (NO) together with its molecular size (115 pm).

Three-dimensional model of NO. Biology[edit] In humans, nitric oxide is produced from L-arginine by three enzymes called nitric oxide synthases (NOS): inducible (iNOS), endothelial (eNOS), and neuronal (nNOS). The latter two are constantly active in endothelial cells and neurons respectively, whereas iNOS' action can be induced in states like inflammation (for example, by cytokines). In inflammation, several cells use iNOS to produce NO, including eosinophils.
Although iNOS is thought to be the main contributor to exhaled NO in asthmatics,[2][3] studies in mice also point to a role for nNOS.[4][5] Airway resistance. Airway resistance is a concept in respiratory physiology that describes the resistance of the respiratory tract to airflow during inspiration and expiration.
Airway resistance can be measured using body plethysmography. Definition[edit] Analogously, to Ohm's Law: Air trapping. Air trapping, also called gas trapping, is an abnormal retention of air in the lungs where it is difficult to exhale completely.[1] It is observed in obstructive lung diseases such as asthma, bronchiolitis obliterans syndrome and chronic obstructive pulmonary diseases such as emphysema and chronic bronchitis.
Air trapping is not a diagnosis but is a presentation of an illness and can be used to find an appropriate diagnosis. Measurement and Function[edit] Exhaled volumes are measured by a pulmonary function test or simple spirometry, leading to an elevated residual volume and a measurement of forced expiratory volume. Closing capacity. See also[edit] Lung volumes Further reading[edit] Rodarte JR, Hyatt RE, Cortese DA (July 1975).
"Influence of expiratory flow on closing capacity at low expiratory flow rates". J Appl Physiol 39 (1): 60–5. Respiratory rate. Measurement[edit] Human respiration rate is measured when a person is at rest and involves counting the number of breaths for one minute by counting how many times the chest rises.
An optical breath rate sensor can be used for monitoring patients during a magnetic resonance imaging scan.[1] Respiration rates may increase with fever, illness, or other medical conditions. When checking respiration, it is important to also note whether a person has any difficulty breathing. Functional residual capacity. Lung Volumes Functional Residual Capacity (FRC) is the volume of air present in the lungs, specifically the parenchyma tissues, at the end of passive expiration.
At FRC, the elastic recoil forces of the lungs and chest wall are equal but opposite and there is no exertion by the diaphragm or other respiratory muscles. FRC is the sum of Expiratory Reserve Volume (ERV) and Residual Volume (RV) and measures approximately 2400 mL in a 70 kg, average-sized male. It can not be estimated through spirometry, since it includes the residual volume. In order to measure RV precisely, one would need to perform a test such as nitrogen washout, helium dilution or body plethysmography. Hypoxicator. A hypoxicator is a medical device intended to provide a stimulus for the adaptation of an individual's cardiovascular system by means of breathing reduced oxygen hypoxic air and triggering mechanisms of compensation.

The aim of intermittent hypoxic training or hypoxic therapy conducted with such a device is to obtain benefits in physical performance and wellbeing through improved oxygen metabolism. There are several commercial systems available, the most popular being Hypoxico, Inc., who pioneered normobaric hypoxic altitude training systems.
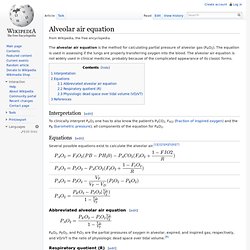
Most of these systems have not been cleared for medical applications by the FDA and are used by athletes for altitude training. Alveolar air equation. The alveolar air equation is the method for calculating partial pressure of alveolar gas (PAO2).
Respiratory sounds. Respiratory sounds, breath sounds, or lung sounds refer to the specific sounds generated by the movement of air through the respiratory system.

These may be easily audible or identified through auscultation of the respiratory system through the lung fields[1] with a stethoscope. These include normal breath sounds and adventitious or "added" sounds such as rales, wheezes, pleural friction rubs, stertor and stridor. Alveolar pressure. Alveolar pressure (Palv) is the pressure in centimeters of water pressure (cmH2O) held within the alveoli of the lungs during inspiration.[1] The pressure value is the difference from atmospheric pressure, which is considered zero when establishing the value. Jump up ^ Sondergaard S, Kárason S, Hanson A, Nilsson K, Wiklund J, Lundin S et al. (2003). "The dynostatic algorithm accurately calculates alveolar pressure on-line during ventilator treatment in children. ". Paediatr Anaesth 13 (4): 294–303. doi:10.1046/j.1460-9592.2003.01064.x. PMID 12753441. Hypercapnia.
Hypercapnia or hypercapnea (from the Greek hyper = "above" or "too much" and kapnos = "smoke"), also known as hypercarbia, is a condition of abnormally elevated carbon dioxide (CO2) levels in the blood. Carbon dioxide is a gaseous product of the body's metabolism and is normally expelled through the lungs. Hypercapnia normally triggers a reflex which increases breathing and access to oxygen, such as arousal and turning the head during sleep. CO₂ retention. CO2 retention is a pathophysiological process in which too little carbon dioxide is removed from the blood by the lungs. The end result is hypercapnia, an elevated level of carbon dioxide dissolved in the bloodstream. Various diseases may lead to this state; disturbed gas exchange may lead to impaired excretion of the gas.
In addition, breathing air with a high carbon dioxide concentration may also lead to hypercapnia. Hypoxic pulmonary vasoconstriction. The process might at first seem illogical, as low oxygen levels should theoretically lead to increased blood flow to the lungs to receive increased gaseous exchange. However, it is explained by the fact that constriction leads to redistribution of bloodflow to better-ventilated areas of the lung, which increases the total area involved in gaseous exchange.
This improves ventilation/perfusion ratio and arterial oxygenation, but is less helpful in the case of long-term whole-body hypoxia. This is seen in COPD, at altitude and in heart failure. Several factors inhibit this process including increased cardiac output, hypocapnia, hypothermia, acidosis/alkalosis, increased pulmonary vascular resistance, inhaled anesthetics, calcium channel blockers, positive end-expiratory pressure (PEEP), high-frequency ventilation (HFV), isoproterenol, nitrous oxide, and vasodilators.
Oxygen pulse. Helium dilution technique. The helium dilution technique is the way of measuring the functional residual capacity of the lungs (the volume left in the lungs after normal expiration). Young–Laplace equation. Functional residual capacity. Lung volumes. Oxygen–haemoglobin dissociation curve. Ventilatory threshold. In kinesiology, ventilatory threshold refers to the point during exercise at which ventilation starts to increase at a faster rate than VO2 (V - volume, O2 - oxygen). One’s threshold is said to reflect levels anaerobiosis and lactate accumulation.
As the intensity level of the activity being performed increase, breathing becomes faster; more steadily first and then more rapid as the intensity increases. When breathing surpasses normal ventilation rate, you have reaches ventilatory threshold. For most people this threshold lies at exercise intensities between 50% and 75% of VO2 max. Rapid shallow breathing index. DLCO.