

Rapid shallow breathing index. Hypoxic pulmonary vasoconstriction. The process might at first seem illogical, as low oxygen levels should theoretically lead to increased blood flow to the lungs to receive increased gaseous exchange.
However, it is explained by the fact that constriction leads to redistribution of bloodflow to better-ventilated areas of the lung, which increases the total area involved in gaseous exchange. This improves ventilation/perfusion ratio and arterial oxygenation, but is less helpful in the case of long-term whole-body hypoxia. This is seen in COPD, at altitude and in heart failure. Several factors inhibit this process including increased cardiac output, hypocapnia, hypothermia, acidosis/alkalosis, increased pulmonary vascular resistance, inhaled anesthetics, calcium channel blockers, positive end-expiratory pressure (PEEP), high-frequency ventilation (HFV), isoproterenol, nitrous oxide, and vasodilators.
Valsalva maneuver. The Valsalva maneuver or Valsalva manoeuvre is performed by moderately forceful attempted exhalation against a closed airway, usually done by closing one's mouth, pinching one's nose shut while pressing out as if blowing up a balloon. Variations of the maneuver can be used either in medical examination as a test of cardiac function and autonomic nervous control of the heart, or to "clear" the ears and sinuses (that is, to equalize pressure between them) when ambient pressure changes, as in diving, hyperbaric oxygen therapy, or air travel. The technique is named after Antonio Maria Valsalva,[1] a 17th-century physician and anatomist from Bologna whose principal scientific interest was the human ear. He described the Eustachian tube and the maneuver to test its patency (openness).
He also described the use of this maneuver to expel pus from the middle ear. A modified version is done by expiring against a closed glottis. Arteriovenous oxygen difference. The arteriovenous oxygen difference, or a-vO2 diff, is the difference in the oxygen content of the blood between the arterial blood and the venous blood.

It is an indication of how much oxygen is removed from the blood in capillaries as the blood circulates in the body. The a-vO2 diff and cardiac output are the main factors that allow variation in the body's total oxygen consumption, and are important in measuring VO2. Halorespiration. Halorespiration or dehalorespiration is the use of halogenated compounds as terminal electron acceptors in anaerobic respiration.[1] Halorespiration can play a part in microbial biodegradation.

The most common substrates are chlorinated aliphatics (PCE, TCE), chlorinated phenols. Dehalorespiring bacteria are highly diverse. This trait is found in some proteobacteria, chloroflexi (green nonsulfur bacteria) and low G+C gram positive Clostridia.[2] Jump up ^ Holliger, C.; Wohlfarth, G.; Diekert, G. (1998). Rapid shallow breathing index. Closing capacity. See also[edit] Lung volumes Further reading[edit] Rodarte JR, Hyatt RE, Cortese DA (July 1975).
"Influence of expiratory flow on closing capacity at low expiratory flow rates". J Appl Physiol 39 (1): 60–5. Pneumograph. A pneumograph, also known as a pneumatograph or spirograph, is a device for recording velocity and force of chest movements during respiration.
Principle of operation[edit] There are various kinds of pneumographic devices, which have different principles of operation. Discontinuous gas exchange. Oxygen–haemoglobin dissociation curve. The oxygen–hemoglobin dissociation curve plots the proportion of hemoglobin in its saturated form on the vertical axis against the prevailing oxygen tension on the horizontal axis.

The oxyhemoglobin dissociation curve is an important tool for understanding how our blood carries and releases oxygen. Specifically, the oxyhemoglobin dissociation curve relates oxygen saturation (sO2) and partial pressure of oxygen in the blood (pO2), and is determined by what is called "Hemoglobin affinity for oxygen"; that is, how readily hemoglobin acquires and releases oxygen molecules into the fluid that surrounds it. Background[edit] Hemoglobin (Hb), a globular protein, is the primary vehicle for transporting oxygen in the blood.
Oxygen is also carried dissolved in the blood's plasma, but to a much lesser degree. Hemoglobin is contained in erythrocytes, more commonly referred to as red blood cells. Sigmoidal shape[edit] File:Oxyhemoglobin dissociation curve.png Hemoglobin saturation curve. Note: Functional residual capacity. Lung Volumes.
Respiratory examination. Respiratory examination In medicine, the respiratory examination is performed as part of a physical examination,[1] or when a patient presents with a respiratory problem (dyspnea (shortness of breath), cough, chest pain) or a history that suggests a pathology of the lungs.
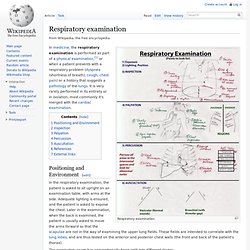
It is very rarely performed in its entirety or in isolation, most commonly it's merged with the cardiac examination. Positioning and Environment[edit] In the respiratory examination, the patient is asked to sit upright on an examination table, with arms at the side. Adequate lighting is ensured, and the patient is asked to expose the chest. Oxygen saturation in medicine. Oxygen saturation[edit] Haemoglobin saturation curve.
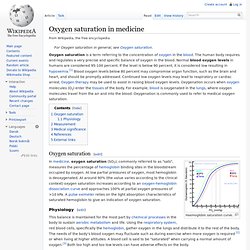
In medicine, oxygen saturation (SO2), commonly referred to as "sats", measures the percentage of hemoglobin binding sites in the bloodstream occupied by oxygen. At low partial pressures of oxygen, most hemoglobin is deoxygenated. Airway resistance. Airway resistance is a concept in respiratory physiology that describes the resistance of the respiratory tract to airflow during inspiration and expiration.
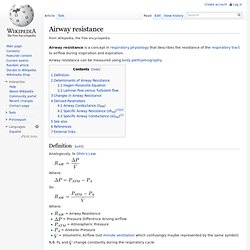
Airway resistance can be measured using body plethysmography. Definition[edit] Analogously, to Ohm's Law: Where: So: = Airway Resistance = Pressure Difference driving airflow = Atmospheric Pressure = Alveolar Pressure = Volumetric Airflow (not minute ventilation which confusingly maybe represented by the same symbol) N.B. Helium dilution technique. VD/VT. Equation[edit] References[edit] Jump up ^ Raymond LW (1978). "The alveolar air equation abbreviated. ". Chest 74 (6): 675–6. PMID 738126. FEV1/FVC ratio. The FEV1/FVC ratio, also called Tiffeneau-Pinelli[1] index, is a calculated ratio used in the diagnosis of obstructive and restrictive lung disease.[2][3] It represents the proportion of a person's vital capacity that they are able to expire in the first second of expiration.[4] See the Wikipedia article on spirometry for the definitions of FEV1 and FVC.
Normal values are approximately 80%.[5] Predicted normal values can be calculated online and depend on age, sex, height, mass and ethnicity as well as the research study that they are based upon. A derived value of FEV1% is FEV1% predicted, which is defined as FEV1% of the patient divided by the average FEV1% in the population for any person of similar age, sex and body composition. Rapid shallow breathing index. Alveolar air equation. Respiratory gas humidification. Respiratory rate. Closing capacity. Peak expiratory flow.
The peak expiratory flow (PEF), also called peak expiratory flow rate (PEFR) is a person's maximum speed of expiration, as measured with a peak flow meter, a small, hand-held device used to monitor a person's ability to breathe out air. Postural drainage. Drainage used in bronchiectasis and lung abscess. Bronchial challenge test. Exhaled nitric oxide. Chemical formula of nitric oxide (NO) together with its molecular size (115 pm). Three-dimensional model of NO. Peak inspiratory pressure. Pulmonary function testing. Pulmonary Function Testing (PFT) is a complete evaluation of the respiratory system including patient history, physical examinations, chest x-ray examinations, arterial blood gas analysis, and tests of pulmonary function. Bohr effect. Hemoglobin Dissociation Curve.
United States Army Pike's Peak Research Laboratory. Intrapleural pressure. Ventilation/perfusion scan. Rapid shallow breathing index. List of terms of lung size and activity. Bronchial challenge test. Respiration (physiology) Ventilation (physiology) Anaerobic respiration. High-pressure nervous syndrome. Halcyon RB80. Hydrogen narcosis. Nitrogen narcosis. Blood oxygen level. Timeline of respiratory therapy. Gas exchange. Carbon dioxide data. Respiratory physiology. Continuous positive airway pressure. Anaerobic respiration. High-frequency ventilation. Modes of mechanical ventilation. Table of modes of mechanical ventilation. Fraction of inspired oxygen. Spirometry. Atmospheric pressure. CO₂ retention. Decompression sickness. Lung volumes. Pulmonary gas pressures. Partial pressure.