

Epidemiology and Pathophysiology of Aplastic Anemia. Epidemiology of Aplastic Anemia The incidence of aplastic anemia (AA) in Europe and North America is approximately 2 per million population and is about 2-3 times higher in East Asia.1,2 There is a biphasic age distribution with peaks at 10-25 years and > 60 years.2 There is no significant difference in incidence between men and women.2 Did You Know...?
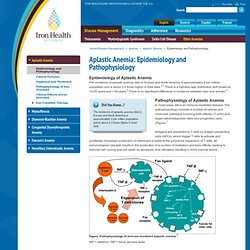
The incidence of aplastic anemia (AA) in Europe and North America is approximately 2 per million population and is about 2-3 times higher in East Asia. Pathophysiology of Aplastic Anemia In most cases, AA is an immune-mediated disease. Antigens are presented to T cells by antigen-presenting cells (APCs), which trigger T cells to activate and proliferate. Figure. INF = interferon; TNF = tumor necrosis factor. Variations in the clinical presentation and in patients' response to therapy are probably due to genetic risk factors, exposure to environmental factors, and individual differences in the immune response. Pathophysiologic Mechanisms in Acquired Aplastic Anemia. Historically, patients with severe forms of marrow failure have faced a dismal prognosis, and there are formidable practical difficulties of experimentation in a rare disorder in which the cells of interest have disappeared.
Early observers of the disease emphasized putative etiologies and the relationship of aplastic anemia to environmental factors, such as chemicals (especially benzene) and idiosyncratically to specific medical drug exposures (most notably chloramphenicol). Over several decades, and following on the observations of improvement of blood counts in the majority of patients who were treated with immunosuppressive therapies, understanding of aplastic anemia has cohered around a unified immune mechanism of hematopoietic cell destruction.
Technical advances in cell biology, flow cytometry, molecular biology, and immunology provided methods to measure numbers and function of very limited numbers of cells. Etiologies Clinical associations Epidemiology Autoantigens Pathophysiology. B Cells and T Cells. Lymphocytes are one of the five kinds of white blood cells or leukocytes), circulating in the blood.
[More] Although mature lymphocytes all look pretty much alike, they are extraordinarily diverse in their functions. The most abundant lymphocytes are: B lymphocytes (often simply called B cells) and T lymphocytes (likewise called T cells). B cells are produced in the bone marrow. The precursors of T cells are also produced in the bone marrow but leave the bone marrow and mature in the thymus (which accounts for their designation). Each B cell and T cell is specific for a particular antigen. The specificity of binding resides in a receptor for antigen: Cell-mediated immunity. In the previous sections, we described mechanisms of humoral immunity.
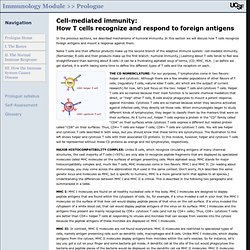
In this section we will discuss how T cells recognize foreign antigens and mount a response against them. Naïve T cells and their effector products make up the second branch of the adaptive immune system: cell-mediatd immunity. (Remember, B cells and their products make up the first branch: humoral immunity.) Learning about T cells tends to feel less straightforward than learning about B cells—it can be a frustrating alphabet soup of terms, (CD, MHC, HLA…) so before we get started, it is worth taking some time to define the different types of T cells and the receptors on each.
THE CD NOMENCLATURE: For our purposes, T lymphocytes come in two flavors: helper and cytotoxic. MHC I: MHC I molecules are found on all healthy nucleated cells in the body. MHC II: In contrast, MHC II molecules are not found everywhere. The image below is meant to help summarize and review the properties of MHC I and MHC II molecules. Immunology Overview (recent and good summary)
Evolution of the Immune System The immune system consists of factors that provide innate and acquired immunity, and has evolved to become more specific, complex, efficient, and regulated. One of the principal functions of the human immune system is to defend against infecting and other foreign agents by distinguishing self from non-self (foreign antigens) and to marshal other protective responses from leukocytes.
The immune system, if dysregulated, can react to self antigens to cause autoimmune diseases or fail to defend against infections. Organization/Components/Functions The immune system is organized into discrete compartments to provide the milieu for the development and maintenance of effective immunity. Cells of the immune system intercommunicate by ligand-receptor interactions between cells and/or via secreted molecules called cytokines.